Bruxism
Bruxism
Abstract:This chapter explores the neurophysiological mechanisms behind bruxism, a condition commonly viewed as an oral parafunctional activity not related to normal functions like eating or speaking. While the literature reports bruxism prevalence ranging from 8% to 31% in the general population, it remains a complex phenomenon often associated with jaw muscle pain, tooth wear, and headaches. There are ongoing debates about whether bruxism is pathological or a physiological function that enhances masticatory capacity, as suggested by the theory of 'Thegosis.'
Through extensive literature analysis, we question whether bruxism is linked to occlusal factors, stress, anxiety syndromes, or trigeminal motoneuron excitability. Studies reveal that while occlusal factors are frequently discussed, little attention has been given to the functionality of the trigeminal nervous system. Research by İnan et al. and Jessica M. D'Amico et al. highlights the role of decreased inhibitory control in trigeminal motoneurons in individuals with bruxism, suggesting a neurophysiological basis for the condition.
The chapter delves into neurobiological mechanisms, examining persistent internal ionic currents (PIC) in the trigeminal motor neuron pool and the influence of serotonin and norepinephrine during micro-awakenings, which are frequent in bruxist individuals. The relationship between drugs affecting neurotransmitter levels and the involuntary activity seen in bruxism is also discussed. However, despite advancements in understanding the neurophysiological aspects, the full pathophysiology of bruxism remains elusive, often presenting as a symptom of broader neuromotor hyperexcitability.
Finally, the chapter presents a clinical case of a 32-year-old patient suffering from severe bruxism for 15 years, emphasizing the need for a thorough differential diagnosis. Using the same clinical roadmap as in the case of hemimasticatory spasm, the chapter offers insights into how the complexities of neurophysiological systems manifest in conditions like bruxism and stresses the importance of integrating a quantum probability model for a more comprehensive understanding.
Introduction to the Bruxism
Let's start by asking ourselves some specific questions:
- Is bruxism an oral parafunctional activity,[1] not physiologically related to normal functions, such as eating or speaking?
- Is bruxism a common behavior despite reports of prevalence ranging from 8% to 31% in the general population?[2]
- Are there any symptoms which are commonly associated with bruxism, including jaw muscle pain, headaches, hypersensitive teeth, tooth wear, and damage to dental restorations (e.g., crowns and fillings)?[3]
Symptoms may be minimal, without the patient being aware of the condition. If no action is taken, after a while many teeth begin to wear out until they disappear completely, the question that arises is:
- do teeth wear out equally in the life cycle even without grinding?
A theory called 'Thegosis' studied by a group of New Zealand researchers[4][5] has always maintained that bruxism is a physiological function that increases masticatory capacity and organic muscle strength, therefore, where is the boundary between physiology and pathology?
These might seem irrelevant questions, but let's see what can be deduced from the literature. There are, of course, multiple factors[6][7] of which many theories are sometimes excessively supported and this is why we questioned Pubmed on specific keywords:
- 'Bruxism'
The query was answered with 1750 results in 10 years[8] and 882 results combining the two keywords 'Bruxism AND sleep bruxism'.[9]- 'Bruxism AND sleep bruxism AND stress' -
We had a dramatic reduction to 96 results[10] which made us wonder if there was an occlusal cause.- 'Bruxism AND sleep bruxism AND occlusal factor'-
We had 32 results[11] that led us to wonder if there were any anxiety-producing causes in the phenomenon.- 'Bruxism AND sleep bruxism AND anxiety syndromes'-
The reduction became more marked with 12 results[12] so that between stress and forms of anxiety we wondered if the phenomenon was somehow attributable to a form of neuro-excitability of the Central Nervous System.- 'Bruxism AND sleep bruxism AND trigeminal motoneuron'
with immense surprise, only two fantastic scientific papers came out: that of İnan R et al.[13] and that of Jessica M D'Amico et al.[14] which we propose as a sub-chapter of Masticationpedia for their important specific scientific contribution on the excitability of trigeminal motor neurons in bruxism.
Substantially, from this overview of the database research it is clear that if on the one hand bruxism is a complex phenomenon on the other the efforts have concentrated almost exclusively on occlusal and dental factors in general, leaving out one aspect, essential in our opinion, that of functionality of the trigeminal nervous system.
Trigeminal motor neuron pool evidences
A synthetic extraction of the contents of the article by Jessica M D'Amico et al.,[14], shows evidence that the discharge of neurons in the raphe nuclei, in the locus coeruleus, in the subcoeruleus and in A5/A7 cells, releases serotonin and norepinephrine and facilitates PIC (persistent internal ionic currents referred to as 'PIC') to the trigeminal motor neuron pool. These episodes increase during micro-awakenings (Leung and Mason 1999,[15] Sakai and Crochet 2001,[16] Takahashi et al., 2010[17]). Individuals with bruxism experience an increase in the number of micro-awakenings during sleep (Kato et al. 2001,[18] 2003,[19] 2011[20]) with a probable increase in the monoaminergic drive towards trigeminal motor neurons. Accordingly, drugs such as serotonin reuptake inhibitors and amphetamines, which increase norepinephrine and serotonin levels, respectively, increase episodes of involuntary activity in bruxist participants (Lavigne et al. 2003,[21] See and Tan 2003[22]) and the amplitude of PICs in motor neurons of the limbs (D'Amico et al. 2013,[23] Udina et al. 2010[24]).
Again on the same neurobiological tenor of GABA and Glutamate, the consideration of Andrisani G.[25] is expressed which leaves everyone somewhat surprised, namely 'the bruxism is not a parafunction, and it functions to activate the ascending reticular formation (ARAS) to regulate the loss of neurotransmitters such as noradrenaline, dopamine, serotonin, acetylcholine and glutamate.
It emerged from another interesting study by M C Verhoeff et al.[26] that although bruxism is present in subjects with Parkinson's this is not associated with the dose of the dopaminergic drug.
While for Merete Bakke et al.[27] exposure to dopamine receptor blocking agents such as antipsychotics, antitussives and antiemetics can induce dystonia including bruxism making the differential diagnosis between similar and possibly related disorders such as Parkinson's disease, essential tremor, Tourette's syndrome, temporomandibular disorders, nocturnal bruxism.
Neurophysiological Conclusion
The conclusion, unfortunately, remains the same and that is that the external manifestation of an organic and/or functional disturbance is a macroscopic effect which transfers a series of mesoscopic abnormalities of the system over time. Here we were able to test only some of these neurobiological mesoscopic phenomena but the clinical result must be interpreted as a whole phenomenon because current scientific knowledge does not allow us to weigh the physiopathological value of the neurotransmitters, the PIC, the basal nuclei, the ascending reticular formation, etc. . What is certain is that an abnormality in one of these sites can generate an 'encrypted code' as a message in machine language of the Central Nervous System which in itself could not be 'Bruxism' but a form of 'Neuromotor Hyperexcitability'.
As usual we are faced with the same problem of vagueness of verbal language as happened with the patient Mary Poppins,the 'Bruxism' may just be a conventional term to be distinguished from an other term such as 'Tremor' but essentially the machine code may not be related to the verbal meaning.
Precisely by following the now acclaimed 'Masticationpedia' model, we are preparing to present a patient suffering from 'Bruxism' for 15 years and whose dental colleagues have obviously seen the significance given to the disorder and consequently managed with an occlusal bite plane.
Also in this clinical case the differential diagnosis, as reported by Merete Bakke et al.,[27] remains very complex.
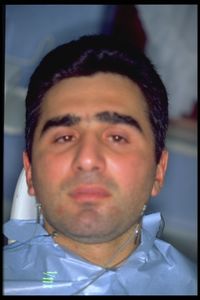
In presenting this clinical case (figure 1), of course, we will follow the same roadmap followed with our patient Mary Poppins suffering from 'Hemimasticatory Spasm'. The subject was a 32-year-old man suffering from pronounced nocturnal and diurnal bruxism and chronic bilateral OP prevalent in the temporoparietal regions, with greater intensity and frequency on the left side.
- ↑ Wassell R, Naru A, Steele J, Nohl F, «Applied occlusion», Quintessence, 2008, London – in «Quintessentials of dental practice».
ISBN: 9781850970989 - ↑ Manfredini D, Winocur E, Guarda-Nardini L, Paesani D, Lobbezoo F, «Epidemiology of bruxism in adults: a systematic review of the literature», in J Orofac Pain, 2013».
PMID:23630682
DOI:10.11607/jop.921 - ↑ Tyldesley WR, Field A, Longman L, «Tyldesley's Oral medicine», Oxford University Press, 2003, Oxford».
ISBN: 978-0192631473 - ↑ Every RG, «The significance of extreme mandibular movements», in Lancet, 1960».
- ↑ Every RG, «The teeth as weapons», in Lancet, 1965».
- ↑ Cawson RA, Odell EW, Porter S, «Cawsonś essentials of oral pathology and oral medicine», Churchill Livingstone, 2002, Edinburgh».
ISBN: 978-0443071065 - ↑ Shetty S, Pitti V, Satish Babu CL, Surendra Kumar GP, Deepthi BC, «Bruxism: a literature review», in J Indian Prosthodont Soc, 2010».
PMID:21886404 - PMCID:3081266
DOI:10.1007/s13191-011-0041-5 - ↑ Bruxism: https://pubmed.ncbi.nlm.nih.gov/?term=bruxism&filter=datesearch.y_10
- ↑ Bruxism AND sleep bruxism. https://pubmed.ncbi.nlm.nih.gov/?term=%27Bruxism+AND+sleep+bruxism+&filter=datesearch.y_10
- ↑ Bruxism AND sleep bruxism AND stress: https://pubmed.ncbi.nlm.nih.gov/?term=%27Bruxism+AND+sleep+bruxism+AND+stress&filter=datesearch.y_10
- ↑ Bruxism AND sleep bruxism AND occlusal factor.https://pubmed.ncbi.nlm.nih.gov/?term=%27Bruxism+AND+sleep+bruxism+AND+occlusal+factor&filter=datesearch.y_10
- ↑ Bruxism AND sleep bruxism AND anxiety syndrome. https://pubmed.ncbi.nlm.nih.gov/?term=%27Bruxism+AND+sleep+bruxism+AND+anxiety+syndromes&filter=datesearch.y_10
- ↑ Rahşan İnan, Gülçin Benbir Şenel, Figen Yavlal, Derya Karadeniz, Ayşegül Gündüz, Meral Erdemir Kızıltan, «Sleep bruxism is related to decreased inhibitory control of trigeminal motoneurons, but not with reticulobulbar system», in Neurol Sci, 2017».
DOI:10.1007/s10072-016-2711-x - ↑ 14.0 14.1 D'Amico Jessica M, Utku Yavuz, Saraçoglu Ahmet, Elif Sibel Atiş, Gorassini Monica Ann, Türker Kemal S, «Activation properties of trigeminal motoneurons in participants with and without bruxism», in J Neurophysiol, 2013».
DOI:10.1152/jn.00536.2013 - ↑ Leung CG, Mason P, «Physiological properties of raphe magnus neurons during sleep and walking», in J Neurophysiol, American Physiological Society, 1999, Rockville, Maryland, USA».
PMID:10036262
DOI:10.1152/jn.1999.81.2.584 - ↑ Sakai K, Crochet S, «Differentiation of presumed serotonergic dorsal raphe neurons in relation to behaviour and wake-sleep states», in Neuroscience, 2001».
PMID:11457597
DOI:10.1016/s0306-4522(01)00103-8 - ↑ Takahashi K, Kayama Y, Lin JS, Sakai K, «Locus coeruleus neuronal activity during the sleep-waking cycle in mice», in Neuroscience, 2010».
PMID:20542093
DOI:10.1016/j.neuroscience.2010.06.009 - ↑ {{cita libro | autore = Kato T | autore2 = Rompre PH | autore3 = Montplaisir JY | autore4 = Sessle BJ | autore5 = Lavigne GJ | titolo = Sleep bruxism: an oromotor activity secondary to microarousal | url = https://pubmed.ncbi.nlm.nih.gov/11706956 | volume = | opera = J Dent Res | anno = 2001 | editore = | città = | ISBN = | DOI = 10.1177/00220345010800101501 | PMID = 11706956 | PMCID = | oaf = | LCCN = | OCLC = }
- ↑ Kato T, Montplaisir JY, Guitard F, Sessle BJ, Lavigne GJ. Evidence that experimentally induced sleep bruxism is a consequence of transient arousal. J Dent Res 82: 284–288, 2003 [PubMed] [Google Scholar]
- ↑ Kato T, Masuda Y, Yoshida A, Morimoto T, «Masseter EMG activity during sleep and sleep bruxism», in Arch Ital Biol, 2011».
PMID:22205593
DOI:10.4449/aib.v149i4.1317 - ↑ Lavigne GJ, Kato T, Kolta A, Sessle BJ, «Neurobiological mechanisms involved in sleep bruxism», in Crit Rev Oral Biol Med, 2003».
PMID:12764018
DOI:10.1177/154411130301400104 - ↑ See SJ, Tan EK, «Case Report: severe amphetamine-induced bruxism: treatment with botulinum toxin», in Acta Neurol Scand, 2003».
PMID:12580870
DOI:10.1034/j.1600-0404.2003.02086.x - ↑ D'Amico JM, Murray KC, Li Y, Chan KM, Finlay MG, Bennett DJ, Gorassini Monica Ann, «Constitutively-active 5HT2/α1 receptors facilitate muscle spasms after human spinal cord injury», in J Neurophysiol, American Physiological Society, 2013, Rockville, Maryland, USA».
- ↑ Udina E, D'Amico J, Bergquist AJ, Gorassini Monica Ann, «Amphetamine increases persistent inward currents in human motoneurons estimated from paired motor unit activity», in J Neurophysiol, American Physiological Society, 2010, Rockville, Maryland, USA».
PMID:20053846 - PMCID:PMC2887628
DOI:10.1152/jn.00734.2009 - ↑ Andrisani Giovanni, Andrisani Giorgia, «The neurophysiological basis of bruxism», in Heliyon, Elsevier, 2021».
PMID:34286138 - PMCID:PMC8273205
DOI:10.1016/j.heliyon.2021.e07477
This is an Open Access resource! - ↑ Verhoeff MC, Koutris M, van Selms MKA, Brandwijk AN, Heres MS, Berendse HW, van Dijk KD, «Is dopaminergic medication dose associated with self-reported bruxism in Parkinson's disease? A cross-sectional, questionnaire-based study», in Clin Oral Investig, 2021».
PMID:32918624 - PMCID:PMC8060196
DOI:10.1007/s00784-020-03566-0 - ↑ 27.0 27.1 Bakke M, Henriksen T, Biernat HB, Dalager T, Møller E, «Interdisciplinary recognizing and managing of drug-induced tardive oromandibular dystonia: two case reports», in Clin Case Rep, John Wiley & Sons Ltd, 2018, Hoboken, New Jersey, USA».
PMID:30455910 - PMCID:PMC6230632
DOI:10.1002/ccr3.1548
This is an Open Access resource!