Difference between revisions of "Influence of the Text Neck Posture on the Static Dental Occlusion"
| Line 65: | Line 65: | ||
A widely debated topic in the literature is whether or not changes in head and neck posture have a significant influence on dental occlusion. However, the effect of ''text neck posture'' (TNP) on occlusion has been overlooked in the dental literature. Chapman et al. (1991) used the T-Scan system to record and analyze the occlusal contacts that occur in ''maximum intercuspation'' (MI) in three different head positions: supine, sitting erect, and sitting with the head tipped forward.<ref>Chapman R.J., Maness W.L., Osorio J. Occlusal contact variation with changes in head position. Int. J. Prosthodont. 1991;4:377–381.</ref> They proved that the mandible is pushed forward during closure when the head is tipped forward, resulting in more anterior initial contacts. However, the total number of occlusal contacts in MI was not significantly modified by the postural change. This means that the main effect of a changed head position was on the initial tooth contacts, which guide the mandible back into MI from eccentric positions. The authors speculated that the location of the first occlusal contacts in the anterior region of the dental arches during closure (i.e., when the head is tipped forward) could produce occlusal overload of the individual teeth. Therefore, they are expected to alter the activity of the elevator muscles. | A widely debated topic in the literature is whether or not changes in head and neck posture have a significant influence on dental occlusion. However, the effect of ''text neck posture'' (TNP) on occlusion has been overlooked in the dental literature. Chapman et al. (1991) used the T-Scan system to record and analyze the occlusal contacts that occur in ''maximum intercuspation'' (MI) in three different head positions: supine, sitting erect, and sitting with the head tipped forward.<ref>Chapman R.J., Maness W.L., Osorio J. Occlusal contact variation with changes in head position. Int. J. Prosthodont. 1991;4:377–381.</ref> They proved that the mandible is pushed forward during closure when the head is tipped forward, resulting in more anterior initial contacts. However, the total number of occlusal contacts in MI was not significantly modified by the postural change. This means that the main effect of a changed head position was on the initial tooth contacts, which guide the mandible back into MI from eccentric positions. The authors speculated that the location of the first occlusal contacts in the anterior region of the dental arches during closure (i.e., when the head is tipped forward) could produce occlusal overload of the individual teeth. Therefore, they are expected to alter the activity of the elevator muscles. | ||
In another T-Scan study of mouth closure, Makofsky et al. (1991) found that in subjects 30 years of age and older, a 30° ventroflexion of the head shifted the initial occlusal contacts anteriorly, while a 45° head extension displaced the contacts posteriorly older.<ref>Makofsky H.W., Sexton T.R., Diamond D.Z., Sexton M.T. The effect of head posture on muscle contact position using the T-Scan system of occlusal analysis. CRANIO® 1991;9:316–321. doi: 10.1080/08869634.1991.11678378.</ref> Gupta et al. (2017) reported that the occlusal contact area in MI varies between two different head postures: 90° upright and 30° ventroflexed [12].<ref>Gupta S., Tarannum F., Gupta N.K., Upadhyay M., Abdullah A. Effect of head posture on tooth contacts in dentate and complete denture wearers using computerized occlusal analysis system. J. Indian Prosthodont. Soc. 2017;17:250–254. doi: 10.4103/jips.jips_321_16.</ref> The pressed occlusal contact area (mm<sup>2</sup>) was measured using the Dental Prescale System (Dental Prescale, Fuji Film Co., Tokyo, Japan), a computerized occlusal analysis system used for the measurement and analysis of the bite force (N), the occlusal contact area (mm2), and the bite pressure (MPa). They concluded that the pressed occlusal contact area (mm<sup>2</sup>) decreased in head ventroflexion compared to the upright-erect position. | In another T-Scan study of mouth closure, Makofsky et al. (1991) found that in subjects 30 years of age and older, a 30° ventroflexion of the head shifted the initial occlusal contacts anteriorly, while a 45° head extension displaced the contacts posteriorly older.<ref name=":3">Makofsky H.W., Sexton T.R., Diamond D.Z., Sexton M.T. The effect of head posture on muscle contact position using the T-Scan system of occlusal analysis. CRANIO® 1991;9:316–321. doi: 10.1080/08869634.1991.11678378.</ref> Gupta et al. (2017) reported that the occlusal contact area in MI varies between two different head postures: 90° upright and 30° ventroflexed [12].<ref>Gupta S., Tarannum F., Gupta N.K., Upadhyay M., Abdullah A. Effect of head posture on tooth contacts in dentate and complete denture wearers using computerized occlusal analysis system. J. Indian Prosthodont. Soc. 2017;17:250–254. doi: 10.4103/jips.jips_321_16.</ref> The pressed occlusal contact area (mm<sup>2</sup>) was measured using the Dental Prescale System (Dental Prescale, Fuji Film Co., Tokyo, Japan), a computerized occlusal analysis system used for the measurement and analysis of the bite force (N), the occlusal contact area (mm2), and the bite pressure (MPa). They concluded that the pressed occlusal contact area (mm<sup>2</sup>) decreased in head ventroflexion compared to the upright-erect position. | ||
Such studies have proved that physiological head positions, which are adopted naturally by the subjects, have a significant influence on some of the investigated static occlusal parameters, including the number and position of the initial tooth contacts during mouth closure, as well as on the occlusal contact area in MI. It must be pointed out that a 30° ventroflexion of the head coincides with the active feeding posture, while a 45° head extension is used for drinking.<ref>Haralur S.B., Al-Gadhaan S.M., Al-Qahtani A.S., Mossa A., Al-Shehri W.A., Addas M.K. Influence of functional head postures on the dynamic functional occlusal parameters. Ann. Med. Health Sci. Res. 2014;4:562–566. doi: 10.4103/2141-9248.139319.</ref> | Such studies have proved that physiological head positions, which are adopted naturally by the subjects, have a significant influence on some of the investigated static occlusal parameters, including the number and position of the initial tooth contacts during mouth closure, as well as on the occlusal contact area in MI. It must be pointed out that a 30° ventroflexion of the head coincides with the active feeding posture, while a 45° head extension is used for drinking.<ref>Haralur S.B., Al-Gadhaan S.M., Al-Qahtani A.S., Mossa A., Al-Shehri W.A., Addas M.K. Influence of functional head postures on the dynamic functional occlusal parameters. Ann. Med. Health Sci. Res. 2014;4:562–566. doi: 10.4103/2141-9248.139319.</ref> | ||
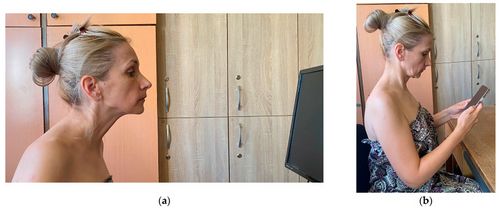
Fewer studies have addressed the effect of abnormal head positions such as the ''forward head posture''(FHP) on dental occlusion. In FHP, the subject pushes her/his head in front of its natural position over the cervical spine, with a simultaneous posterior bending of the head and a compensatory extension of the upper cervical spine, in order to maintain the horizontal direction of the eyes—for example, facing the computer desktop<ref>Patwardhan A.G., Khayatzadeh S., Havey R.M., Voronov L.I., Smith Z.A., Kalmanson O., Ghanayem A.J., Sears W. Cervical sagittal balance: A biomechanical perspective can help clinical practice. Eur. Spine J. 2018;27:25–38. doi: 10.1007/s00586-017-5367-1.</ref> (Figure 1a). Some authors even call this the desktop neck posture.<ref>(accessed on 20 July 2022)]. Available online: [https://erikdalton.com/blog/text-neck-desktop-neck/ <nowiki>https://erikdalton.com/blog/text-neck-desktop-neck [Ref list]</nowiki>]</ref> | Fewer studies have addressed the effect of abnormal head positions such as the ''forward head posture''(FHP) on dental occlusion. In FHP, the subject pushes her/his head in front of its natural position over the cervical spine, with a simultaneous posterior bending of the head and a compensatory extension of the upper cervical spine, in order to maintain the horizontal direction of the eyes—for example, facing the computer desktop<ref>Patwardhan A.G., Khayatzadeh S., Havey R.M., Voronov L.I., Smith Z.A., Kalmanson O., Ghanayem A.J., Sears W. Cervical sagittal balance: A biomechanical perspective can help clinical practice. Eur. Spine J. 2018;27:25–38. doi: 10.1007/s00586-017-5367-1.</ref> (Figure 1a). Some authors even call this the desktop neck posture.<ref>(accessed on 20 July 2022)]. Available online: [https://erikdalton.com/blog/text-neck-desktop-neck/ <nowiki>https://erikdalton.com/blog/text-neck-desktop-neck [Ref list]</nowiki>]</ref> | ||
[[File:Stoica 1.jpeg|center|thumb|500x500px|'''Figure 1:''' ('''a''') Forward head posture (FHP), which is sometimes called the desktop neck posture; ('''b''') text neck posture (TNP)—examples given by one of the examiners in the study.]] | |||
In a sample of thirty-nine normal subjects, Makofsky (2000) did not find a significant relationship between experimentally induced FHP and the initial occlusal contact pattern that occured while the subject was slowly and completely biting onto the sensor of the T-Scan II Occlusal Diagnostic System.<ref>Makofsky H.W. The influence of forward head posture on dental occlusion. CRANIO® 2000;18:30–39. doi: 10.1080/08869634.2000.11746111.</ref> This result is of interest because the same author proved in a previous study that the initial occlusal contact pattern during closure is influenced by the extension of the head.<ref name=":3" /> It appears that in FHP, which involves a significant degree of head and upper cervical spine extension, the alteration in the mandibular position is not important enough to produce the occlusal changes observed during a physiological head extension. This conclusion has clinical relevance in the treatment of patients with ''temporo-mandibular disorders'' (TMD) and FHP. Some authors claim a relationship between FHP and TMD.<ref>Lee W.Y., Okeson J.P., Lindroth J. The relationship between forward head posture and temporomandibular disorders. J. Orofac. Pain. 1995;9:161–167.</ref><ref>Huggare J.A., Raustia A.M., Makofsky H.W. Head posture and cervicovertebral and craniofacial morphology in patients with craniomandibular dysfunction. CRANIO® 1992;10:173–179. doi: 10.1080/08869634.1992.11677908.</ref> If the initial occlusal contact pattern does not change in FHP, that means that the occlusion is not an etiological factor of the TMD and should not be therapeutically addressed. | |||
It must be pointed out that FHP is different from the TNP (as pointed out in Figure 1), although they are often incorrectly used as synonyms. Assumed while using a smartphone, the TNP is characterized by a flexed position of the upper cervical region, with the eyes facing downward and fixed on the smartphone<ref name=":0" />—Figure 1b. | |||
Following the impact of this aspect on today’s population, as well as the shortcomings of the literature on this topic, as pointed out above, the aim of this study was to investigate the influence of TNP on static occlusion in young healthy subjects with normal occlusal relationships. | |||
=== Materials and Methods === | |||
The present study was conducted according to the guidelines of the Declaration of Helsinki. It was approved by CECS no. 70/22.12.2021 of the Ethical Committee of the “Victor Babes” University of Medicine and Pharmacy of Timisoara, Romania. | |||
==== Study Subjects ==== | |||
A total of nineteen subjects, fifteen females and four males (aged 20 to 24 years), were considered for this research. This sample was chosen for convenience. The process of consecutive selection among young subjects who were interested in a free examination of their masticatory system was based on the following inclusion criteria: full dental arches (except for the third molars in some subjects); normal values of overbite (2 to 4 mm) and overjet (1 to 2 mm); Angle Class I occlusion, without posterior crossbite; healthy periodontal status, with normal physiological tooth mobility; no signs and symptoms of TMD; no pain or limited range of motion in the cervical spine. | |||
In addition, all standing subjects were able to adopt a ''normal head posture'' (NHP), with the head and back straight and with the external auditory meatus on the same vertical line as the acromio-clavicular joint (i.e., the shoulder), the hip, and the knee. Their head was placed in the midline, with the chin above the manubrium, while their neck had a slight lordotic curve and a normal length, without tilting or rotation of the head.<ref name=":4">Ombregt L. A system of Orthopaedic Medicine. 3rd ed. Churchill Livingstone Elsevier; London, UK: 2013. Clinical Evaluation of the cervical spine; pp. 119–133.</ref> | |||
The exclusion criteria were: degenerative or inflammatory spine pathology; fibro-myalgia; cervical spine traumatic events; autoimmune diseases; and neurologic diseases that can have an impact on cervical position. Furthermore, we excluded subjects that currently reported any of the following parafunctions, which can influence the head and neck position by muscle hyperactivity: awake and/or sleep bruxism; nail biting; biting of the cheeks and lips; ventral position during sleep; keeping the phone between the face and the shoulder; playing violin or a wind instrument; maintaining a pencil between the dental arches; tongue pressing on the lingual surfaces of teeth; abusive consumption of chewing gum.<ref>Okeson J.P. Management of Temporo-Mandibular Disorders and Occlusion. 7th ed. The Mosby Imprint of Elsevier Inc.; St. Louis, MI, USA: 2013. Etiology of functional disturbances in the masticatory system; pp. 102–128.</ref> | |||
The anamnesis and clinical examination of the masticatory system was based on Schiffman’s “Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications”.<ref>Schiffman E., Ohrbach R. Executive summary of the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications. J. Am. Dent. Assoc. 2016;147:438–445. doi: 10.1016/j.adaj.2016.01.007. </ref> The examination of the cervical area was based on the protocol recommended by Ombregt.<ref name=":4" /> | |||
All subjects were fully informed about the nature of the investigation and signed an informed consent form to participate in this research. | |||
==== Examination Procedure ==== | |||
At the beginning of the procedure, we explained the different steps of the examination to our subjects without giving any details about the purpose or hypotheses of the research. The images in Figure 2 and Figure 3 present one of the examiners as she demonstrates the NHP (Figure 2) and the TNP (Figure 3) to the study subjects. | |||
{{Bib}} | {{Bib}} | ||
Revision as of 14:45, 10 June 2023
| Title | Influence of the Text Neck Posture on the Static Dental Occlusion |
| Authors | Eniko Tunde Stoica^1 · Corina Marcauteanu · Anca Tudor · Virgil-Florin Duma · Elena Constanta Amaricai · Roxana Onofrei · Oana Suciu · Meda Lavinia Negrutiu · Cosmin Sinescu |
| Source | Document |
| Date | 2022 |
| Journal | Medicina (Kaunas) |
| DOI | 10.3390/medicina58091303 |
| PUBMED | https://pubmed.ncbi.nlm.nih.gov/36143980/ |
| PDF copy | |
| License | CC BY |
| This resource has been identified as a Free Scientific Resource, this is why Masticationpedia presents it here as a mean of gratitude toward the Authors, with appreciation for their choice of releasing it open to anyone's access | |
This is free scientific content. It has been released with a free license, this is why we can present it here now, for your convenience. Free knowledge, free access to scientific knowledge is a right of yours; it helps Science to grow, it helps you to have access to Science
This content was relased with a 'CC BY' license.
You might perhaps wish to thank the Author/s
Free resource by Eniko Tunde Stoica^1 · Corina Marcauteanu · Anca Tudor · Virgil-Florin Duma · Elena Constanta Amaricai · Roxana Onofrei · Oana Suciu · Meda Lavinia Negrutiu · Cosmin Sinescu
|
TADERP Research Center, “Victor Babes” University of Medicine and Pharmacy of Timisoara, 9 Revolutiei 1989 Ave., 300070 Timisoara, Romania; moc.oohay@najmedokine
2School of Dental Medicine, “Victor Babes” University of Medicine and Pharmacy of Timisoara, 2A Eftimie Murgu Place, 300070 Timisoara, Romania; or.tfmu@roduta (A.T.); moc.oohay@uiturgen_adem (M.L.N.); moc.liamg@ucsenisonim (C.S.)
3Research Center in Dental Medicine Using Conventional and Alternative Technologies, School of Dental Medicine, “Victor Babes” University of Medicine and Pharmacy of Timisoara, 9 Revolutiei 1989 Ave., 300070 Timisoara, Romania; or.tfmu@anele.iacirama
43OM Optomechatronics Group, Faculty of Engineering, “Aurel Vlaicu” University of Arad, 2 Elena Dragoi Str., 310177 Arad, Romania
5Doctoral School, Polytechnic University of Timisoara, 1 Mihai Viteazu Ave., 300222 Timisoara, Romania
6Department of Rehabilitation, Physical Medicine and Rheumatology, Research Center for Assessment of Human Motion, Functionality and Disability, “Victor Babes” University of Medicine and Pharmacy of Timisoara, 2A Eftimie Murgu Place, 300070 Timisoara, Romania; or.tfmu@anaxor.ierfono (R.O.); or.tfmu@87uicusanao (O.S.)
*Correspondence: moc.oohay@iroc_acram (C.M.); gro.rebmemaso@ligriv.amud (V.-F.D.); Tel.: +40-741-182-478 (C.M.); +40-751-511-451 (V.-F.D.)
Abstract
Background and Objectives: The excessive use of smartphones for various tasks led to a new adverse postural phenomenon called text neck. The aim of this study was to investigate the effect of the text neck posture (TNP) on static occlusion by using the T-Scan III occlusal diagnostic system. Materials and Methods: Nineteen subjects (aged 20 to 24 years) were considered for this research. They had normal values for anterior overbite and overjet, Angle Class I occlusion, no posterior crossbite, and no signs or symptoms of cervical or temporo-mandibular disorders. Occlusal registrations were performed with the T-Scan III system in a normal, neutral head posture (NHP), as well as in the TNP. The investigated parameters were: occlusion time (OT), asymmetry index of the occlusal force (AOF), percent of the maximum movie force (%MMF), and the time elapsed from the last occlusal contact until the maximum intercuspation (MAT-OTB). The last three parameters were analyzed in the maximum area frame (MA) of the registrations. For the statistical analysis of the recorded data, the Wilcoxon Signed Ranks test and the Spearman’s correlation coefficient were used. Results: The following values were obtained in NHP and in TNP: for AOF, 14.88 ± 10.39% and 18.04 ± 12.83%, respectively; for OT, 1.34 ± 1.84 s and 1.32 ± 1.8 s, respectively; for the %MMF, 97.5 ± 2.83% and 96.31 ± 3.17%, respectively; for MAT-OTB, 2.08 ± 1.82 s and 1.45 ± 2.3 s, respectively. There were no statistically significant differences between the static occlusal parameters measured in NHP and those in TNP. However, the high values of the AOF and OT in NHP revealed an imbalance of the occlusal force distribution between the right and left side in maximum intercuspation (MI), as well as a lack of simultaneity of static occlusal contacts. Furthermore, there was a significant, direct, and strong correlation between OT and AOF in NHP. Conclusions: The NHP should not be used as the starting position in TNP simulations in T-Scan studies, so as to avoid statistically insignificant differences between static occlusion in NHP and TNP. The healthy standing subjects, with normal occlusal relationships from the clinical point of view, revealed an occlusal instability in NHP when examined with the T-Scan.
Keywords: text neck posture (TNP), static occlusion, maximum intercuspation (MI), T-Scan III system, occlusion time (OT), asymmetry index of the occlusal force (AOF)
Introduction
The term text neck was proposed by a chiropractor, Dr. Dean L. Fishman,[1] and it is used to define both a bad postural position and a syndrome associated with the prolonged and inappropriate use of handheld mobile devices, including smartphones.[2][3][4] This adverse postural phenomenon can be described as a sustained flexed neck position, with the head tilted forward. It is associated with forward-rolled shoulders, which increase the curve of the thoracic spine. [2][4] Compared to the neutral posture, the higher neck flexion angle requires an increased activity of the neck muscles in order to compensate for the effect of gravity.[5] These biomechanical changes in the cervical and thoracic spine, as well as muscular imbalances and postural compensations, finally lead to cervical muscle fatigue and pain. [2][3]
The scientific literature demonstrates that any change in the head and neck posture induces a change in the rest position of the mandible,[6] in the activity of the masticatory muscles,[7] and in the habitual path of mouth closing.[8] In an interesting study, Yamada et al. (1999) found that as the head bended forward (i.e., in ventroflexion), the closing path approached the maximum intercuspation position (MIP) from the anterior region.[9] The forward bending of the head also decreased the stability of the closing path. On the other hand, as the head was bent backward, the closing path approached the MIP from the posterior region and its stability increased.
A widely debated topic in the literature is whether or not changes in head and neck posture have a significant influence on dental occlusion. However, the effect of text neck posture (TNP) on occlusion has been overlooked in the dental literature. Chapman et al. (1991) used the T-Scan system to record and analyze the occlusal contacts that occur in maximum intercuspation (MI) in three different head positions: supine, sitting erect, and sitting with the head tipped forward.[10] They proved that the mandible is pushed forward during closure when the head is tipped forward, resulting in more anterior initial contacts. However, the total number of occlusal contacts in MI was not significantly modified by the postural change. This means that the main effect of a changed head position was on the initial tooth contacts, which guide the mandible back into MI from eccentric positions. The authors speculated that the location of the first occlusal contacts in the anterior region of the dental arches during closure (i.e., when the head is tipped forward) could produce occlusal overload of the individual teeth. Therefore, they are expected to alter the activity of the elevator muscles.
In another T-Scan study of mouth closure, Makofsky et al. (1991) found that in subjects 30 years of age and older, a 30° ventroflexion of the head shifted the initial occlusal contacts anteriorly, while a 45° head extension displaced the contacts posteriorly older.[11] Gupta et al. (2017) reported that the occlusal contact area in MI varies between two different head postures: 90° upright and 30° ventroflexed [12].[12] The pressed occlusal contact area (mm2) was measured using the Dental Prescale System (Dental Prescale, Fuji Film Co., Tokyo, Japan), a computerized occlusal analysis system used for the measurement and analysis of the bite force (N), the occlusal contact area (mm2), and the bite pressure (MPa). They concluded that the pressed occlusal contact area (mm2) decreased in head ventroflexion compared to the upright-erect position.
Such studies have proved that physiological head positions, which are adopted naturally by the subjects, have a significant influence on some of the investigated static occlusal parameters, including the number and position of the initial tooth contacts during mouth closure, as well as on the occlusal contact area in MI. It must be pointed out that a 30° ventroflexion of the head coincides with the active feeding posture, while a 45° head extension is used for drinking.[13]
Fewer studies have addressed the effect of abnormal head positions such as the forward head posture(FHP) on dental occlusion. In FHP, the subject pushes her/his head in front of its natural position over the cervical spine, with a simultaneous posterior bending of the head and a compensatory extension of the upper cervical spine, in order to maintain the horizontal direction of the eyes—for example, facing the computer desktop[14] (Figure 1a). Some authors even call this the desktop neck posture.[15]
In a sample of thirty-nine normal subjects, Makofsky (2000) did not find a significant relationship between experimentally induced FHP and the initial occlusal contact pattern that occured while the subject was slowly and completely biting onto the sensor of the T-Scan II Occlusal Diagnostic System.[16] This result is of interest because the same author proved in a previous study that the initial occlusal contact pattern during closure is influenced by the extension of the head.[11] It appears that in FHP, which involves a significant degree of head and upper cervical spine extension, the alteration in the mandibular position is not important enough to produce the occlusal changes observed during a physiological head extension. This conclusion has clinical relevance in the treatment of patients with temporo-mandibular disorders (TMD) and FHP. Some authors claim a relationship between FHP and TMD.[17][18] If the initial occlusal contact pattern does not change in FHP, that means that the occlusion is not an etiological factor of the TMD and should not be therapeutically addressed.
It must be pointed out that FHP is different from the TNP (as pointed out in Figure 1), although they are often incorrectly used as synonyms. Assumed while using a smartphone, the TNP is characterized by a flexed position of the upper cervical region, with the eyes facing downward and fixed on the smartphone[2]—Figure 1b.
Following the impact of this aspect on today’s population, as well as the shortcomings of the literature on this topic, as pointed out above, the aim of this study was to investigate the influence of TNP on static occlusion in young healthy subjects with normal occlusal relationships.
Materials and Methods
The present study was conducted according to the guidelines of the Declaration of Helsinki. It was approved by CECS no. 70/22.12.2021 of the Ethical Committee of the “Victor Babes” University of Medicine and Pharmacy of Timisoara, Romania.
Study Subjects
A total of nineteen subjects, fifteen females and four males (aged 20 to 24 years), were considered for this research. This sample was chosen for convenience. The process of consecutive selection among young subjects who were interested in a free examination of their masticatory system was based on the following inclusion criteria: full dental arches (except for the third molars in some subjects); normal values of overbite (2 to 4 mm) and overjet (1 to 2 mm); Angle Class I occlusion, without posterior crossbite; healthy periodontal status, with normal physiological tooth mobility; no signs and symptoms of TMD; no pain or limited range of motion in the cervical spine.
In addition, all standing subjects were able to adopt a normal head posture (NHP), with the head and back straight and with the external auditory meatus on the same vertical line as the acromio-clavicular joint (i.e., the shoulder), the hip, and the knee. Their head was placed in the midline, with the chin above the manubrium, while their neck had a slight lordotic curve and a normal length, without tilting or rotation of the head.[19]
The exclusion criteria were: degenerative or inflammatory spine pathology; fibro-myalgia; cervical spine traumatic events; autoimmune diseases; and neurologic diseases that can have an impact on cervical position. Furthermore, we excluded subjects that currently reported any of the following parafunctions, which can influence the head and neck position by muscle hyperactivity: awake and/or sleep bruxism; nail biting; biting of the cheeks and lips; ventral position during sleep; keeping the phone between the face and the shoulder; playing violin or a wind instrument; maintaining a pencil between the dental arches; tongue pressing on the lingual surfaces of teeth; abusive consumption of chewing gum.[20]
The anamnesis and clinical examination of the masticatory system was based on Schiffman’s “Diagnostic Criteria for Temporomandibular Disorders (DC/TMD) for Clinical and Research Applications”.[21] The examination of the cervical area was based on the protocol recommended by Ombregt.[19]
All subjects were fully informed about the nature of the investigation and signed an informed consent form to participate in this research.
Examination Procedure
At the beginning of the procedure, we explained the different steps of the examination to our subjects without giving any details about the purpose or hypotheses of the research. The images in Figure 2 and Figure 3 present one of the examiners as she demonstrates the NHP (Figure 2) and the TNP (Figure 3) to the study subjects.
- ↑ Neupane S., Ali U.I., Mathew A. Text neck syndrome-systematic review. Imp. J. Interdiscip. Res. 2017;3:141–148. [Google Scholar] [Ref list]
- ↑ 2.0 2.1 2.2 2.3 Fiebert I., Kistner F., Gissendanner C., DaSilva C. Text neck: An adverse postural phenomenon. Work. 2021;69:1261–1270. doi: 10.3233/WOR-213547.
- ↑ 3.0 3.1 Cuéllar J.M., Lanman T.H. “Text neck”: An epidemic of the modern era of cell phones? Spine J. 2017;17:901–902. doi: 10.1016/j.spinee.2017.03.009.
- ↑ 4.0 4.1 Moreno M.A., Hoopes A.J. Technology and Adolescent Health: In Schools and Beyond.Academic Press; Cambridge, MA, USA: 2020. The impact of digital media; p. 367.
- ↑ Ailneni R.C., Syamala K.R., Kim I.S., Hwang J. Influence of the wearable posture correction sensor on head and neck posture: Sitting and standing workstations. Work. 2019;62:27–35. doi: 10.3233/WOR-182839
- ↑ Darling D.W., Kraus S., Glasheen-Wray M.B. Relationship of head posture and the rest position of the mandible. J. Prosthet. Dentistry. 1984;52:111–115. doi: 10.1016/0022-3913(84)90192-6
- ↑ Boyd C.H., Slagle W.F., Boyd C.M., Bryant R.W., Wiygul J.P. The effect of head position on electromyographic evaluations of representative mandibular positioning muscle groups. CRANIO® 1987;5:50–54. doi: 10.1080/08869634.1987.11678174.
- ↑ Goldstein D.F., Kraus S.L., Willams W.B., Glasheen-Wray M. Influence of cervical posture on mandibular movement. J. Prosthet. Dent. 1984;52:421–426. doi: 10.1016/0022-3913(84)90460-8.
- ↑ Yamada R., Ogawa T., Koyano K. The effect of head posture on direction and stability of mandibular closing movement. J. Oral Rehabil. 1999;26:511–520. doi: 10.1046/j.1365-2842.1999.00386.x.
- ↑ Chapman R.J., Maness W.L., Osorio J. Occlusal contact variation with changes in head position. Int. J. Prosthodont. 1991;4:377–381.
- ↑ 11.0 11.1 Makofsky H.W., Sexton T.R., Diamond D.Z., Sexton M.T. The effect of head posture on muscle contact position using the T-Scan system of occlusal analysis. CRANIO® 1991;9:316–321. doi: 10.1080/08869634.1991.11678378.
- ↑ Gupta S., Tarannum F., Gupta N.K., Upadhyay M., Abdullah A. Effect of head posture on tooth contacts in dentate and complete denture wearers using computerized occlusal analysis system. J. Indian Prosthodont. Soc. 2017;17:250–254. doi: 10.4103/jips.jips_321_16.
- ↑ Haralur S.B., Al-Gadhaan S.M., Al-Qahtani A.S., Mossa A., Al-Shehri W.A., Addas M.K. Influence of functional head postures on the dynamic functional occlusal parameters. Ann. Med. Health Sci. Res. 2014;4:562–566. doi: 10.4103/2141-9248.139319.
- ↑ Patwardhan A.G., Khayatzadeh S., Havey R.M., Voronov L.I., Smith Z.A., Kalmanson O., Ghanayem A.J., Sears W. Cervical sagittal balance: A biomechanical perspective can help clinical practice. Eur. Spine J. 2018;27:25–38. doi: 10.1007/s00586-017-5367-1.
- ↑ (accessed on 20 July 2022)]. Available online: https://erikdalton.com/blog/text-neck-desktop-neck [Ref list]
- ↑ Makofsky H.W. The influence of forward head posture on dental occlusion. CRANIO® 2000;18:30–39. doi: 10.1080/08869634.2000.11746111.
- ↑ Lee W.Y., Okeson J.P., Lindroth J. The relationship between forward head posture and temporomandibular disorders. J. Orofac. Pain. 1995;9:161–167.
- ↑ Huggare J.A., Raustia A.M., Makofsky H.W. Head posture and cervicovertebral and craniofacial morphology in patients with craniomandibular dysfunction. CRANIO® 1992;10:173–179. doi: 10.1080/08869634.1992.11677908.
- ↑ 19.0 19.1 Ombregt L. A system of Orthopaedic Medicine. 3rd ed. Churchill Livingstone Elsevier; London, UK: 2013. Clinical Evaluation of the cervical spine; pp. 119–133.
- ↑ Okeson J.P. Management of Temporo-Mandibular Disorders and Occlusion. 7th ed. The Mosby Imprint of Elsevier Inc.; St. Louis, MI, USA: 2013. Etiology of functional disturbances in the masticatory system; pp. 102–128.
- ↑ Schiffman E., Ohrbach R. Executive summary of the Diagnostic Criteria for Temporomandibular Disorders for clinical and research applications. J. Am. Dent. Assoc. 2016;147:438–445. doi: 10.1016/j.adaj.2016.01.007.