Association between posterior unilateral functional crossbite and asymmetrical spinal flexion: A prospective study
| Title | Association between posterior unilateral functional crossbite and asymmetrical spinal flexion: A prospective study |
| Authors | Maria Grazia Piancino · Giada Matacena · Umberto Garagiola · Farhad B. Naini · Alessandro Tortarolo · David Wertheimf |
| Source | Document |
| Date | 2023 |
| Journal | Heliyon |
| DOI | 10.1016/j.heliyon.2023.e14342 |
| PUBMED | https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10011000/ |
| PDF copy | |
| License | CC BY |
| This resource has been identified as a Free Scientific Resource, this is why Masticationpedia presents it here as a mean of gratitude toward the Authors, with appreciation for their choice of releasing it open to anyone's access | |
This is free scientific content. It has been released with a free license, this is why we can present it here now, for your convenience. Free knowledge, free access to scientific knowledge is a right of yours; it helps Science to grow, it helps you to have access to Science
This content was relased with a 'CC BY' license.
You might perhaps wish to thank the Author/s
Free resource by Maria Grazia Piancino · Giada Matacena · Umberto Garagiola · Farhad B. Naini · Alessandro Tortarolo · David Wertheimf
|
Department of Surgical Sciences, Dental School, University of Turin, Turin, Italy, via Nizza 230, 10126, Turin, Italy
Orthodontist, Private Practice, Turin, Italy
Department of Biomedical Surgical and Dental Sciences, Maxillo-facial and Odontostomatology Unit, Fondazione IRCCS Cà Granda, Ospedale Maggiore Policlinico, University of Milan, Milan, Italy
Consultant Orthodontist, Kingston and St. George's, University Hospitals, NHS Foundation Trust, London, UK
Department of Surgical Sciences, Dental School, University of Turin, Turin, Italy
Faculty of Sciences, Engineering and Computing, Kingston University, Surrey, UK
Maria Grazia Piancino: ti.otinu@onicnaip.aizargairam; Giada Matacena: ti.oohay@anecatam.adaig; Umberto Garagiola: ti.iminu@aloigarag.otrebmu; Farhad B. Naini: ku.oc.oohay@inian.dahraf; Alessandro Tortarolo: ti.otinu@oloratrot.ordnassela; David Wertheim: ku.ca.notsgnik@miehtrew.d
∗Corresponding author. ti.otinu@onicnaip.aizargairam
Abstract
Unilateral posterior crossbite (UPC) with functional shift is a malocclusion that may have the potential to affect the masticatory function and the flexibility of the spine due to intrinsic occlusal, structural and functional asymmetries sustained by marked asymmetrical muscular activation.
Research question
To investigate whether the presence of UPC with functional shift is associated with reverse chewing pattern and altered spine flexion.
Methods
Patients with UPC and a control group of patients with normal occlusion were recorded when chewing soft and hard boluses using a Kinesiograph (Myotronics-Noromed Inc., USA) and spine alignment was assessed with an electronic inclinometer Spinal Mouse® system (Idiag AG, Switzerland).
Results
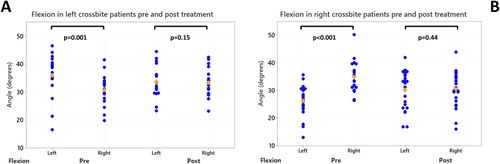
There were 87 children with UPC in the patients' group among whom 38, with median (IQR) age 8.0 (7.3–9.3) years, had measurements before and after treatment. The UPC patients showed a higher percentage of anomalous/reverse chewing patterns on the crossbite side compared with a control group (p < 0.001). Moreover, a clear difference was observed between left and right flexion angles of the spine in the patients’ group (p < 0.001 and p = 0.001, paired t-test) with the crossbite side being more flexible compared to the non-crossbite side. No such differences were seen in the control group, nor post-treatment for right and left crossbite (p = 0.44 and p = 0.15 respectively, paired t-test).
Significance
This study suggests an association between UPC, asymmetrical chewing patterns and asymmetrical flexion of the spine. These results may help improve understanding of any association between dental malocclusions and spine posture and hence aid diagnosis and treatment strategies.
Keywords: Musculoskeletal physiological phenomena, Posture, Spine, Mastication, Chewing, Malocclusion, Crossbite
Introduction
The relationship between dental occlusion/malocclusion and body flexibility, range of motion (ROM) and posture is still a controversial topic. Even though past review papers did not find enough evidence in support of this association, [1][2][3] a few studies have shown that patients with posterior crossbite may have an increased risk of developing spine asymmetries [4][5][6][7][8]and the influence of occlusion on the cervical spine has been substantiated.[9] However, a recent systematic review concluded that there was no clear evidence of a causal relationship between spinal deformities and malocclusions[10] and underlined the limited extent of the literature to date. On the other hand, even though the results are not directly translatable to humans, three interesting animal studies,[11][12][13] showed the role of an induced malocclusion on scoliotic irreversible curve degeneration. Also, the demonstration of possible associations of standard orthodontic therapies, such as rapid palatal expansion, on the worsening of scoliotic curves casts a shadow of concern that requires objective scientific clarification.[14]
The type of malocclusion that may have the potential to influence spinal curvatures due to intrinsic asymmetry is unilateral posterior crossbite (UPC) with functional shift, which is defined as an irregular bucco-lingual or bucco-palatal relationship between opposing teeth, resulting in a lateral displacement of the mandible in order to achieve maximum intercuspation of the dentition during functions.[15] The prevalence of posterior crossbite varies from 8 to 20% depending on the population and the research protocol,[16][17] with more than half being UPC. The presence of posterior crossbite is associated with reduced maxillary growth: depending on the degree of transverse discrepancy between the upper and lower jaws, unilateral or bilateral posterior crossbite may be expressed. Interestingly, the presence of UPC has been associated with dento-alveolar compensation on the non-crossbite side, whereas no significant dento-alveolar compensation was shown in bilateral posterior crossbite (BPC).[18] UPC was also shown to have a significant impact on masticatory function, establishing anomalous reverse chewing patterns during chewing on the crossbite side.[19][20][21][22][23][24][25] Reverse chewing cycles (also known as reverse-sequencing patterns) occur when the direction of the closing trace is inverted: they are characterized by an abnormal, narrow kinematic pattern in the frontal plane, with possible cross-over of the opening and closing tracings, as well as limited lateral displacement of the mandible.[26][27][28][29][30][31][32][33] The result is a serious asymmetry of the masticatory function. Such functional asymmetry is sustained by marked asymmetrical muscular activation between sides[34] which, if not corrected with adequate early therapy, may induce asymmetrical basal growth.[29][35] It is therefore of interest to investigate the relationship between masticatory asymmetry in UPC and asymmetrical flexion of the spine.
Non-invasive devices can be used to evaluate spine posture in children with crossbite without scoliosis or spine pathologies of orthopedic interest.[36] The position and the movement of vertebrae can be accurately imaged with roentgenography (spinal column radiograph), which is the gold standard diagnostic investigation when orthopedic treatment is required. However, the use of X-ray imaging in such studies should be avoided, particularly in children, in view of the radiation exposure with such techniques. A computer-aided device (Spinal Mouse®, Idiag, Voletswil, Switzerland) has been developed to measure the lumbar, thoracic, and sacral spinal curvature with range of motion in the sagittal and frontal planes thus avoiding X-ray imaging, using bone anatomical reference points. The Spinal Mouse is a wheeled electronic inclinometer with accelerometer; the device is directed along a bone anatomical landmark, i.e. vertebral spinous processes and registers distance and changes of spinal movement and inclination.[37] The Spinal Mouse system has been shown to have good intra-rater and inter-rater reliability[38] and can help in the evaluation of motion capability and symmetry.
The aim of this study is to investigate whether the presence of unilateral posterior crossbite with functional shift is associated with reverse chewing pattern and degree of spine flexibility in children with the malocclusion. The null hypothesis (H0) for this study is that unilateral posterior crossbite is not associated with reverse chewing pattern and degree of spine flexibility.
Materials and methods
Patients with unilateral posterior crossbite and a control group of patients with normal occlusion, referred to the Orthodontic Department, Dental School, University of Turin, Italy were consecutively selected from April 2017 through July 2021. Before entering this prospective study, patients and their parents were informed about the aims of the study and the procedures, and the parents signed an informed consent to permit participation. The study was approved by the Institutional Review Board of the University Hospital “Health and Science Complex Turin-Italy” n. CS/246, in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for research involving humans. This study has been planned following the STROBE protocol.
Subjects
The inclusion criteria for the Patients Group were unilateral posterior crossbite (UPC) of two or more posterior teeth with lateral displacement/functional shift, mixed dentition and age less than 14 years for the first study assessment. The exclusion criteria were the presence of previous orthodontic therapy, erupting teeth, caries, dental pain, orthopedic trauma or impairments, back pain, signs or symptoms of dental or myofascial disorders, motor or neurological problems, diabetes and/or celiac disease, spine pathologies, congenital and hereditary pathologies. The Control Group (CG) was carefully selected for normal occlusion without crossbite. Participants were selected on the basis of occlusal diagnosis, performed by an experienced Orthodontist (MPG) by analyzing model casts.
All participants underwent the following sequence of investigations, before treatment (T0) and after treatment (T1)
- clinical and orthodontic examination
- intra- and extra-oral photograph
- model cast
- recording of chewing patterns
- recording of spinal flexion with the Spinal Mouse
The measurements and examinations were conducted in the morning in a dedicated quiet room. The two operators taking Spinal Mouse measurements and masticatory patterns had more than eight years of experience in the use of the instruments; they were unaware of the whether the patient was in the case or control group as well as the purpose of the study. All included patients received functional treatment with the removable appliance Function Generating Bite.[20] The appliance was individually manufactured in acrylic resin and stainless steel, with metallic bite planes made of special resilient steel positioned between the upper and lower dental arches. The action of these bite planes results in mandibular disengagement, levelling of the occlusal plane and prevention of dental prematurities during orthodontic tooth movement. The appliance was designed and activated according to each patient's orthodontic needs.
Kinematic analysis – chewing patterns recording
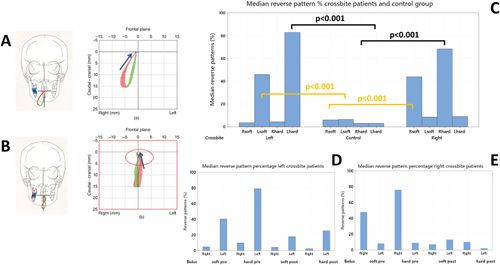
Mandibular motion was tracked using a Kinesiograph (K7–I; Myotronics, Tukwila, WA, USA) that measures jaw movements with an accuracy of 0.1 mm. Multiple Hall effect sensors mounted in an array of weight 113 g were used to track the motion of a tiny magnet attached at the lower interincisor point.[39] The Kinesiograph was interfaced with a computer for data storage and subsequent analysis. The kinematic analysis was carried out separately with a soft and a hard bolus. Recording procedure and signal analysis (Fig. 1) were performed following a standardized, previously published method.[19][20][34]
Spinal mouse recording
Spine alignment in the frontal plane was assessed with an electronic inclinometer Spinal Mouse® system (Idiag, Volestwil, Switzerland); the system consists of a hand-held computer-assisted electromechanical device that can be used to evaluate spinal curvatures in various postures. This is a wheeled device housing accelerometers which records distance and changes of inclination with regard to the plumb line as it is rolled along the length of the spine (effectively, an electronic inclinometer) (Spinal Mouse®) (Idiag, Voletswil, Switzerland). The device is guided by hand along the midline of the spine starting at the spinous process of C7 and finishing at the top of the anal crease at approximately S3 level.
The landmarks are firstly determined by palpation and marked on the skin surface with a cosmetic pencil. Two rolling wheels follow the contour of the spine, and distance and angle measures are communicated via an analog-digital converter from the device to a base station positioned approximately 1–2 m away and interfaced to a personal computer. Data is sampled every 1.3 mm as the mouse traverses along the spine. This information is then used to calculate the relative positions of the sacrum and vertebral bodies of the underlying bony spinal column using an intelligent recursive algorithm. For each testing position, the thoracic (T1-2 to T11-12) angle, lumbar (T12-L1 to the sacrum) spine angle, the trunk inclination angle (angle formed by the vertical and a line joining C7 to the sacrum) and the position of the sacrum and the hips (difference between the sacral angle and the vertical) were recorded.[38] The repeatability and reliability of Spinal Mouse recordings have previously been assessed.[37][40][41][42]
The testing procedure was performed in three different positions, in the following order:
- Standing upright: the subject assumed a relaxed position, with the head looking forward, the arms hanging by the side, the knees normally extended and the feet shoulder-width apart.
- Maximal left-lateral flexion: the subject was asked to slowly flex the trunk laterally to the left as far as comfortably possible, without turning either the shoulders or pelvis.
- Maximal right-lateral flexion: the subject was asked to slowly flex the trunk laterally to the right as far as comfortably possible, without turning either the shoulders or pelvis.
The following spinal parameters were measured:
- General inclination (degrees).
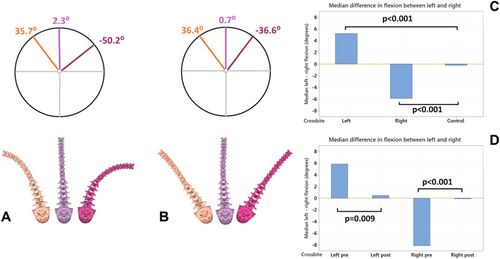
- Bending in the frontal plane (left conventionally expressed as a positive angle and right negative angle; see Fig. 2).
Statistical analysis
Results from the investigations were stored in spreadsheet files using Excel (Microsoft Corporation, USA) and analyzed using Excel and Minitab v19 (Minitab LLC, USA). Data were tested for consistency with a normal distribution using the Ryan-Joiner test in Minitab and parametric or non-parametric tests used as appropriate. A p-value <0.05 was taken to indicate a significant difference.
Results
102 UPC patients were potentially eligible for this study; 15 did not complete the exams (5 the chewing analysis, 10 the postural analysis) and were therefore excluded.
Measurements were recorded from 87 patients with UPC (44 males) with median (IQR) age of 9.1 (7.7–10.6) years, for 51 of whom the crossbite was on the right side. Of the 87 patients with crossbite, 38 (17 males) had measurements both pre (T0) and post (T1) treatment; in this group, 22 patients had right crossbite; the median time difference (IQR) between pre and post treatment assessments (T0/T1) was 1.8 (1.3–2.9) years. In addition, there were 53 children (28 male) in the control group with no crossbite with median (IQR) age of 10.7 (9.3–12.8) years. Of the 53 children in the control group, 35 (19 males) had a second set of measurements (T1) at a median (IQR) of 7 (6–8) months after the first set.
A summary of descriptive statistics from the patients with two assessments is shown in Table 1. For those children, at the first recording (T0) the median (IQR) age of the children overall with crossbite was 8.0 (7.3–9.3) years of age and for the control group 11.1 (9.3–13.0) years of age (p < 0.001, Mann-Whitney test). The first weight assessment was 28 (24–33) kg and for height 132 (126–138) cm in crossbite patients and for the 35 children in the control group, the first weight assessment median (IQR) was 39 (29–45) kg and for height 145 (134–158) cm.
Table 1Summary descriptive statistics from the patients with paired data and control patients. Age, weight and height descriptive statistics for patients with pre and post treatment assessment data as well as the control group. T0: before treatment; T1: after treatment; UPC: unilateral posterior functional crossbite group; Control: control group. Q1-Q3: interquartile range.
|
The pre/post evaluation (T0/T1) was performed to assess the equivalence of the control group with the post treatment group. The crossbite correction was obtained with a functional therapy with Function Generating Bite.[20]
The patients’ group showed a higher percentage of anomalous/reverse chewing patterns during chewing on the crossbite side when chewing soft and hard boluses (Fig. 1a and b and Table 2a) with significant differences in reverse chewing percentages on the side of the crossbite when compared with the equivalent side for control group p < 0.001 (Mann-Whitney test); low percentages of reverse patterns were seen in the control group (Fig. 1c). In addition, there was higher percentage of anomalous/reverse chewing patterns pre-treatment (T0) during chewing on the crossbite side; low percentages of reverse patterns were seen post-treatment (T1) (Fig. 1d and e).
Table 2(a) Descriptive statistics for percentage reverse chewing pattern. Median (Q1-Q3: interquartile range) percentage reverse chewing pattern in left and right crossbite patients as well and the control group. (b) Median (Q1-Q3: interquartile range) Left – Right flexion difference in pre-treatment crossbite patients and first measurement in the control group.
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
For the complete pre-treatment (T0) crossbite group, when comparing the left and right flexion angle difference compared with the control group (Fig. 2, Fig. 3 and Table 2b) there was a significant difference for left and right crossbite patient both being p < 0.001 (Mann-Whitney test), the crossbite side being more flexible compared to the non-crossbite side.
Significant differences between pre and post treatment (T0/T1) were seen in the crossbite patients’ group for difference in left and right flexion angle (Wilcoxon paired test, p = 0.009 left crossbite and p < 0.001 right crossbite) with the crossbite side being more flexible compared to the non-crossbite side as seen in Fig. 3a.
As seen in Fig. 3b, for patients with right and left crossbite there was a clear difference between left and right flexion angles pre-treatment (T0; p < 0.001 and p = 0.001, paired t-test) with the crossbite side being more flexible compared to the non-crossbite side. No such differences were seen post-treatment (T1) for right and left crossbite (p = 0.44 and p = 0.15 respectively, paired t-test). In the control group there was no significant difference between left flexion and right flexion (first assessment p = 0.88 and second assessment p = 0.10, Wilcoxon paired test).
Discussion
This study aimed to investigate the potential influence of unilateral posterior crossbites (UPC) with functional shifts on the masticatory function and spine flexion of affected children. This asymmetric malocclusion is known to alter the masticatory function [20][32]establishing asymmetrical kinematics and an asymmetrical muscular activation between sides.[20][34] No data have been published to date regarding the flexibility of the column. The results show clear differences between the crossbite group and the control group for both chewing patterns and flexion of the spine.
Regarding masticatory function, the chewing patterns of the crossbite group showed a higher percentage of anomalous and reversed chewing cycles during chewing on the crossbite side compared to the non-crossbite side, especially during chewing a hard bolus. There was no clear difference in the percentage of reverse chewing patterns between either side in the control group, nor after treatment (T0/T1) in the crossbite patients.
Posterior crossbite in the mixed dentition is a serious malocclusion that poses significant clinical challenges. It has been suggested that during growth the stomatognathic system compensates the malocclusion to obtain the best function;[43][44] in turn dental occlusion influences function.[45] Because UPC develops during eruption of the primary dentition, it has an influence on the developing central motor control establishing the reverse sequencing type of chewing pattern.[30] Also, as described in the introduction, unilateral posterior crossbite alters the kinematic of the mandible and the coordination of the masticatory muscles during chewing on the crossbite side. In the absence of effective treatment, a severe functional asymmetry is established, which may lead to skeletal asymmetries, irreversible when maturity is reached.[46] The related important muscular asymmetry[20] is likely to correlate with the most nearby muscles of the spine.
Indeed, the lateral spine flexion of the crossbite group showed significant differences between sides, being the crossbite side more flexible. Non-significant differences were observed in the control group. After functional UPC correction treatment (T1), both the chewing patterns and the spine flexibility were consistent with what would be expected in symmetry and seen in the control group. Interestingly, the effects of functional treatment of UPC were not restricted to the symmetrisation of the masticatory function after the correction of the malocclusion but extended as far as the re-balancing of spinal flexion between the sides. More research is needed to clarify the chain of causality at work and the clinical implications of these results.
Nevertheless, these results suggest that mandibular position, rather than a single tooth or teeth alone, affects the dynamic range of movement of the spine. UPC is a dental malocclusion that alters relationships in the three x, y and z spatial planes[45] requiring complex compensation that involves functional alteration and muscular activation. Not all malocclusions are able to alter masticatory function in such an important way. If we think of the mandible as linked to the spine, it is conceivable that it plays a synergistic role with the spine, especially when an asymmetrical function disturbs the balance of the system. The relationship between the masticatory muscles and the muscles of the neck during chewing is known[47]and could explain the muscular reaction of the spinal column muscles to the presence of UPC, which was shown to influence both masticatory patterns the spinal curvatures. These children were not affected by a structural asymmetry of the spine, but by a functional imbalance.
The awareness of the relationship between malocclusion and spine dynamics may be helpful to highlight the importance of the multidisciplinary approach to therapies, especially during development.
In a recent study by Zurita-Hernandez et al., no significant association between untreated UPC in adult subjects and postural alterations was found.[48] This study is interesting, but the postural evaluations were performed with a photographic protocol and static postural platform.
A limitation of our study is the lack of radiographic imaging, which remains the gold standard for assessment of postural deformities, but this would raise ethical issues due to exposure to radiation in children.
As mentioned in the Introduction, bilateral posterior crossbite (BPC) patients may display a less asymmetrical mastication compared to UPC. However, there is little information in the literature concerning the prevalence of RCCs in BPC patients. As a future direction of this research, it would be interesting to investigate the masticatory function and the postural balance in BPC patients, and to research this topic further by assessing vertebral alignment and spine flexibility in untreated adult UPC patients.
Conclusions
This study suggests the association between unilateral posterior crossbite and asymmetrical flexion of the spine, increased on the crossbite side, as well asymmetrical chewing patterns.
Author contribution
Maria Grazia Piancino: Conceived and designed the experiments; Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper
Giada Matacena: Performed the experiments.
Umberto Garagiola; Farhad B. Naini: Conceived and designed the experiments; Wrote the paper.
Alessandro Tortarolo; David Wertheim: Analyzed and interpreted the data; Wrote the paper.
Funding statement
Prof. Maria Grazia Piancino was supported by Ministero dell’Istruzione, dell’Università e della Ricerca [Ex60% 2020].
Data availability statement
Data will be made available on request.
Financial/benefit disclosure statement(s)
This work was funded in part by the Italian Ministry of Education, University and Research, “Ex60% 2020”. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgements
The authors would like to thank dr. Laura Dibenedetto for her precious contribution to the recording of the chewing patterns.
- ↑ Perinetti G. Dental occlusion and body posture: no detectable correlation. Gait Posture. 2006;24(2):165–168
- ↑ Manfredini D., Castroflorio T., Perinetti G., Guarda-Nardini L. Dental occlusion, body posture and temporomandibular disorders: where we are now and where we are heading for. J. Oral Rehabil. 2012;39(6):463–471.
- ↑ Gomes Lde C., Horta K.O., Gonçalves J.R., Santos-Pinto A.D. Systematic review: craniocervical posture and craniofacial morphology. Eur. J. Orthod. 2014;36(1):55–66.
- ↑ O'Byrn B.L., Sadowsky C., Schneider B., BeGole E.A. An evaluation of mandibular asymmetry in adults with unilateral posterior crossbite. Am. J. Orthod. Dentofacial Orthop. 1995;107(4):394–400.
- ↑ Lippold C., Danesh G., Hoppe G., Drerup B., Hackenberg L. Sagittal spinal posture in relation to craniofacial morphology. Angle Orthod. 2006;76(4):625–631.
- ↑ Korbmacher H., Koch L., Eggers-Stroeder G., Kahl-Nieke B. Associations between orthopaedic disturbances and unilateral crossbite in children with asymmetry of the upper cervical spine. Eur. J. Orthod. 2007;29(1):100–104.
- ↑ Hong J.Y., W Suh S., N Modi H., Yang J.H., Hwang Y.C., Lee D.Y., Hur C.Y., Park Y.H. Correlation between facial asymmetry, shoulder imbalance, and adolescent idiopathic scoliosis. Orthopedics. 2011;34(6):187.
- ↑ Primozic J., Perinetti G., Zhurov A., Richmond S., Ovsenik M., Antolic V., Primozic J. Three-dimensional assessment of back symmetry in subjects with unilateral functional crossbite during the pre-pubertal growth phase: a controlled study. Eur. J. Orthod. 2019;41:250–257.
- ↑ Michelotti A., Manzo P., Farella M., Martin R. [Occlusion and posture: is there evidence of correlation?] Minerva Stomatol. 1999;48(11):525–534.
- ↑ Langella F., Fusini F., Rossi G., Villafañe J.H., Migliaccio N., Donzelli S., Berjano P. Spinal deformity and malocclusion association is not supported by high-quality studies: results from a systematic review of the literature. Eur. Spine J. 2019;28(7):1638–1651.
- ↑ D'Attilio M., Filippi M.R., Femminella B., Festa F., Tecco S. The influence of an experimentally-induced malocclusion on vertebral alignment in rats: a controlled pilot study. Cranio. 2005;23(2):119–129.
- ↑ Ramirez-Yanez G.O., Mehta L., Mehta N.R. The effect of dental occlusal disturbances on the curvature of the vertebral spine in rats. Cranio. 2015;33(3):217–227.
- ↑ D'Attilio M., Cesaretti G., Viganò P., Alí Apaza Alccayhuaman K., Botticelli D., Ricardo Silva E., Porfirio X.S. Effects of induced malocclusion on vertebral alignment in rats: a controlled study by CBCTs. Animals (Basel) 2021;11(10):2808.
- ↑ Piancino M.G., MacDonald F., Laponte I., Cannavale R., Crincoli V., Dalmasso P. Juvenile/adolescent idiopathic scoliosis and rapid palatal expansion. A pilot study. Children. 2021;8(5):362.
- ↑ Daskalogiannakis J., Ross R.B., Tompson B.D. The mandibular catch-up growth controversy in Pierre Robin sequence. Am. J. Orthod. Dentofacial Orthop. 2001;120(3):280–285.
- ↑ Thilander B., Lennartsson B. A study of children with unilateral posterior crossbite, treated and untreated, in the deciduous dentition - occlusal and skeletal characteristics of significance in predicting the long-term outcome. J. Orofac. Orthop. 2002;63(5):371–383.
- ↑ Harrison J.E., Ashby D. Orthodontic treatment for posterior crossbites, cochrane database syst. Rev. 1. Cochrane Database Syst. Rev. 8 (2014) CD000979. 2001:CD000979.
- ↑ Miner R.M., Al Qabandi S., Rigali P.H., Will L.A. Cone-beam computed tomography transverse analysis. Part I: normative data. Am. J. Orthod. Dentofacial Orthop. 2012;142(3):300–307.
- ↑ 19.0 19.1 Piancino M.G., Comino E., Talpone F., Vallelonga T., Frongia G., Bracco P. Reverse-sequencing chewing patterns evaluation in anterior versus posterior unilateral crossbite patients. Eur. J. Orthod. 2012;34(5):536–541.
- ↑ 20.0 20.1 20.2 20.3 20.4 20.5 20.6 Piancino M.G., Falla D., Merlo A., Vallelonga T., de Biase C., Dalessandri D., Debernardi C. Effects of therapy on masseter activity and chewing kinematics in patients with unilateral posterior crossbite. Arch. Oral Biol. 2016;67:61–67
- ↑ Ferrario V.F., Piancino M.G., Dellavia C., Castroflorio T., Sforza C., Bracco P. Quantitative analysis of the variability of unilateral chewing movements in young adults. Cranio. 2006;24(4):274–282.
- ↑ Troelstrup B., Moller E. Electromyography of the temporalis and masseter muscles in children with unilateral cross-bite. Scand. J. Dent. Res. 1970;78(5):425–430.
- ↑ Ingervall B., Thilander B. Activity of temporal and masseter muscles in children with a lateral forced bite. Angle Orthod. 1975;45(4):249–258.
- ↑ Michler L., Bakke M., Møller E. Graphic assessment of natural mandibular movements. J. Craniomandib. Disord. 1987;1(2):97–114.
- ↑ Alarcón J.A., Martín C., Palma J. Effect of unilateral posterior crossbite on the electromyographic activity of human masticatory muscles. Am. J. Orthod. Dentofacial Orthop. 2000;118(3):328–334.
- ↑ Lewin A. Quintessence; Berlin: 1985. Electrognathographics. An Atlas for Diagnostic Procedures and Interpretation.
- ↑ Ben-Bassat Y., Yaffe A., Brin I., Freeman J., Ehrlich Y. Functional and morphological-occlusal aspects in children treated for unilateral posterior cross-bite. Eur. J. Orthod. 1993;15(1):57–63.
- ↑ Brin I., Ben-Bassat Y., Blustein Y., Ehrlich J., Hochman N., Marmary Y., Yaffe A. Skeletal and functional effects of treatment for unilateral posterior crossbite. Am. J. Orthod. Dentofacial Orthop. 1996 Feb;109(2):173–179
- ↑ 29.0 29.1 Pinto A.S., Buschang P.H., Throckmorton G.S., Chen P. Morphological and positional asymmetries of young children with functional unilateral posterior crossbite. Am. J. Orthod. Dentofacial Orthop. 2001;120(5):513–520.
- ↑ 30.0 30.1 Throckmorton G.S., Buschang B.H., Hayasaki H., Phelan T. The effects of chewing rates on mandibular kinematics. J. Oral Rehabil. 2001;28(4):328–334.
- ↑ Saitoh I., Hayasaki H., Iwase Y., Nakata M. Improvement in jaw motion following treatment of unilateral crossbite in a child with primary dentition: a case report. Cranio. 2002;20(2):129–134
- ↑ 32.0 32.1 Piancino M.G., Talpone F., Dalmasso P., Debernardi C., Lewin A., Bracco P. Reverse-sequencing chewing patterns before and after treatment of children with a unilateral posterior crossbite. Eur. J. Orthod. 2006;28(5):480–484.
- ↑ ever E., Marion L., Ovsenik M. Relationship between masticatory cycle morphology and unilateral crossbite in the primary dentition. Eur. J. Orthod. 2011;33(6):620–627.
- ↑ 34.0 34.1 34.2 Piancino M.G., Farina D., Talpone F., Merlo A., Bracco P. Muscular activation during reverse and non-reverse chewing cycles in unilateral posterior crossbite. Eur. J. Oral Sci. 2009;117(2):122–128
- ↑ Lam P.H., Sadowsky C., Omerza F. Mandibular asymmetry and condylar position in children with unilateral posterior crossbite. Am. J. Orthod. Dentofacial Orthop. 1999;115(5):569–575
- ↑ Piancino M.G., Dalmasso P., Borello F., Cinnella P., Crincoli V., Garagiola U., de Biase C., Tonni I., Matacena G., Deregibus A. Thoracic-lumbar-sacral spine sagittal alignment and cranio-mandibular morphology in adolescents. J. Electromyogr. Kinesiol. 2019;48:169–175.
- ↑ 37.0 37.1 Mannion A.F., Knecht K., Balaban G., Dvorak J., Grob D. A new skin-surface device for measuring the curvature and global and segmental ranges of motion of the spine: reliability of measurements and comparison with data reviewed from the literature. Eur. Spine J. 2004;13(2):122–136.
- ↑ 38.0 38.1 Kellis E., Adamou G., Tzilios G., Emmanouilidou M. Reliability of spinal range of motion in healthy boys using a skin-surface device. J. Manip. Physiol. Ther. 2008;31(8):570–576
- ↑ Jankelson B. Measurement accuracy of the mandibular kinesiograph - a computerized study. J. Prosthet. Dent. 1980;44(6):656–666.
- ↑ Guermazi M., Ghroubi S., Kassis M., Jaziri O., Keskes H., Kessomtini W., Ben Hammouda I., Elleuch M.H. Validité et reproductibilité du Spinal Mouse pour l'étude de la mobilité en flexion du rachis lombaire [Validity and reliability of Spinal Mouse to assess lumbar flexion] Ann. Readapt. Med. Phys. 2006;49(4):172–177
- ↑ Post R.B., Leferink V.J. Spinal mobility: sagittal range of motion measured with the spinal mouse, a new non-invasive device. Arch. Orthop. Trauma Surg. 2004;124(3):187–192.
- ↑ Ripani M., Di Cesare A., Giombini A., Agnello L., Fagnani F., Pigozzi F. Spinal curvature: comparison of frontal measurements with the Spinal Mouse and radiographic assessment. J. Sports Med. Phys. Fit. 2008;48(4):488–494.
- ↑ Moss M.L. Genetics, epigenetics and causation. Am. J. Orthod. 1981;80(4):366–375.
- ↑ Enlow D.H. A morphogenetic analysis of facial growth. Am. J. Orthod. 1966;52(4):283–299
- ↑ 45.0 45.1 Slavicek R. Relationship between occlusion and temporomandibular disorders: implications for the gnathologist. Am. J. Orthod. Dentofacial Orthop. 2011;139(1):10–14.
- ↑ Ugolini A., Agostino P., Silvestrini-Biavati A., Harrison J.E., Batista K.B. Orthodontic treatment for posterior crossbites. Cochrane Database Syst. Rev. 2021;12(12):CD000979.
- ↑ Carlsson G.E. Neuromuscular problems in the orofacial region: aetiology and organic pathology. Int. Dent. J. 1981;31(3):198–201.
- ↑ Zurita-Hernandez J., Ayuso-Montero R., Cuartero-Balana M., Willaert E., Martinez-Gomis J. Relationship between unilateral posterior crossbite and human static body posture. Int. J. Environ. Res. Publ. Health. 2020;17(15):5303.